New Jersey health system with $3 billion in revenue and 8,500+ employees transformed patient access by using better voice technology.
Summary
Parlance partnered with a $3 billion health system in New Jersey to modernize its voice channel and significantly improve patient access, operational efficiency, and staff experience. Despite major digital investments, the organization was overwhelmed by 110,000+ monthly calls, long hold times, and agent burnout. By deploying HIPAA-compliant voice automation, the health system achieved rapid transformation, saving 4,395 agent hours in the first month, reducing call volume to patient access queues, and generating nearly $1M in annual operational savings. Self-service rates increased from 51% to 68%, patient satisfaction soared (NPS 20 → 55), staff retention improved, and brand performance rose nationally. The case study highlights the strategic value of modernizing the voice channel to meet rising consumer expectations and remain competitive against retail-style healthcare disruptors.
Client Success Story: Operational Efficiency Nets Nearly $1M in Annual Savings
The $995 Thousand Dollar Mistake that Healthcare Executives Keep Making…
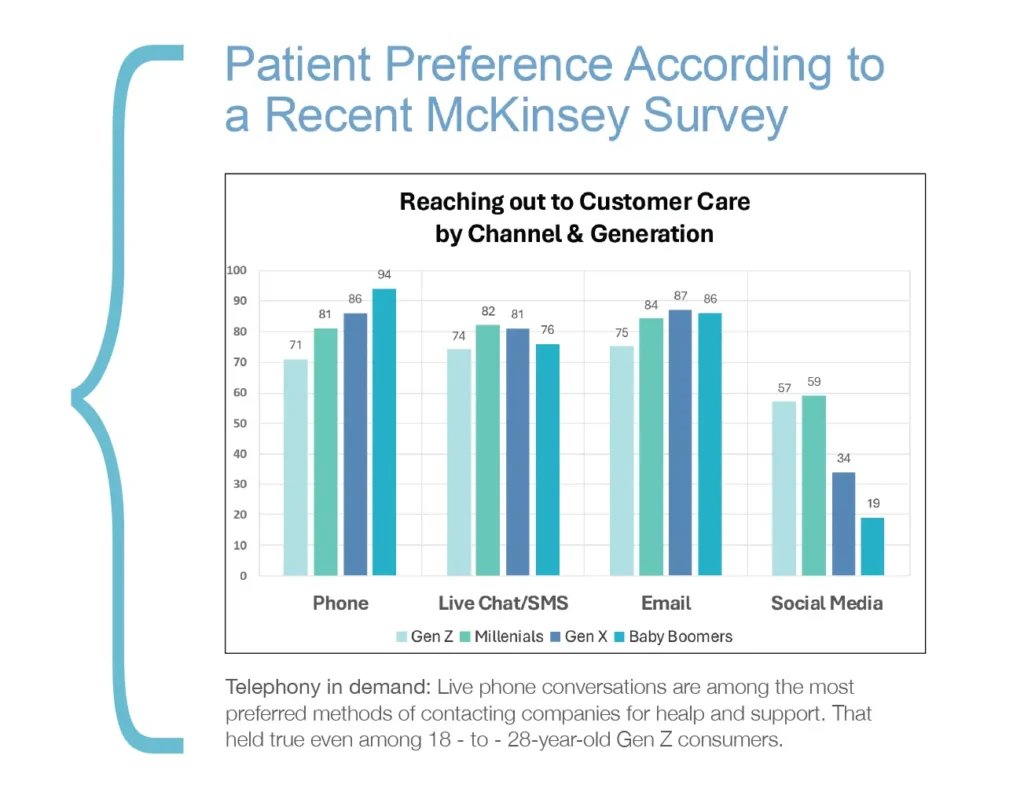
When a small health system in New Jersey decided to tackle their patient access challenges, they discovered something every healthcare executive needs to hear… Don’t assume that younger patients have abandoned the phone — neglecting to modernize the voice channel is costly mistake.
Overview
A $3 billion health system serving New Jersey, with 5 acute care hospitals and over 600 care locations, faced a critical operational challenge that threatened both patient satisfaction and financial performance. Despite major investments in digital transformation initiatives, the patient access center was handling over 110,000 calls monthly, agents were spending significant time transferring calls, and the volume had become a bottleneck rather than an asset.
A healthcare access operations executive dug into the organization’s data and was surprised by what he found.
Challenges
This New Jersey health system’s 250-person access center confronted multiple interconnected operational challenges that demanded urgent attention:
- Operational Inefficiency: Patient access center agents were drowning, spending valuable time on redundant tasks and transfers that prevented them from handling complex patient interactions requiring human expertise. The 110,000 monthly calls were a significant strain on staffing resources.
- Patient Experience Deterioration: Hold times stretched into minutes, leading to patient frustration and abandoned calls. Old-fashioned phone trees created rigid, maze-like experiences that frustrated callers.
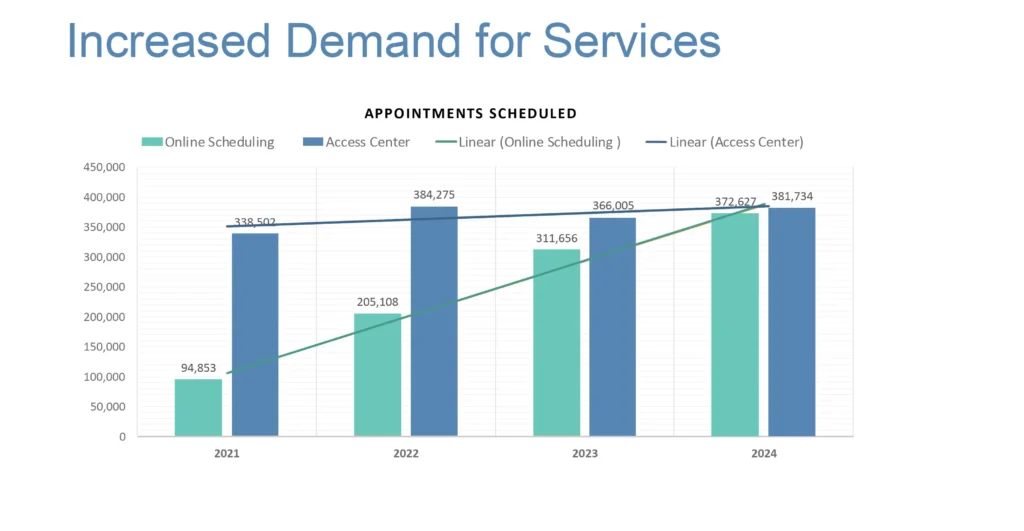
- Generational Expectation Gap: While executives assumed digital adoption would reduce phone demand, the reality proved different. Patients scheduling appointments online still called 2.2 times per appointment for modifications or questions. Online scheduling grew from 94,853 to 372,627 appointments between 2021 and 2024, yet access center volume remained consistently above 375,000 appointments annually.
- Staff Burnout: Operators and agents were experiencing burnout from repetitive tasks and interactions with displeased callers. This was impacting retention and job satisfaction across the patient access center.
- Competitive Vulnerability: As consumer-focused companies like Amazon and CVS entered the healthcare market, this New Jersey health system worried about the risk of losing patients— particularly younger generations with no established provider loyalty—to competitors promising superior healthcare access experiences
The convergence of consumer expectations, competitive pressures, and available technological capabilities created an imperative for immediate action. Executives knew that thier organization could not afford to wait for a perfect solution, when a good solution would deliver measurable results within months. With 60% of hospitals reporting negative margins and rising operational costs across the industry, there was no time to spare.
Solution
The health system implemented a comprehensive voice channel transformation through strategic partnership with Parlance, deploying conversational AI technology that addressed both immediate operational needs and long-term strategic positioning.
Rapid Implementation Approach: The health system committed to a 90-day implementation timeline, recognizing that immediate action was essential to support the brand, given competitive pressures and patient expectations.
Voice Tech Integration: Parlance delivered better self-service rates by enabling callers to speak naturally rather than navigate complex phone trees. The new system could understand patient requests and manage calls appropriately.
True Partnership Model: The collaboration extended beyond typical vendor relationships. One example: when executives requested system modifications during holiday season peak demand on a Friday, the Parlance team implemented changes by Monday morning, demonstrating genuine partnership commitment.
Staff Optimization Strategy: The solution elevated staff capabilities rather than replace personnel, allowing agents and operators to focus on complex interactions genuinely requiring human expertise and empathy. This approach directly addressed the retention challenges plaguing the industry.


Results of Parlance Implementation: Measurable Impact
Financial Performance:
Results: First Month
4,395 agent hours saved (equivalent to 8 FTE reduction)
17% reduction in calls to patient access despite overall demand growth
11% decrease to agent default queue
-
$995,000 in cost savings
-
350% ROI
Patient Satisfaction Transformation
The health system’s Net Promoter Score jumped from 20 to 55, indicating patients transformed from grudgingly tolerating the phone experience to actively recommending the brand to others.
System Capacity Enhancement
Conversational AI enabled an increasing percentage of self-service interactions, growing from 51.5% to 68.2% of all calls.
Brand Performance Impact
The improved patient access experience contributed to the health system’s advancement from 75th to 39th most human-centric healthcare brand nationally in just four years, demonstrating how operational improvements translate to market positioning.
Staff Satisfaction Enhancement
Reduced operator burnout and enhanced job satisfaction resulted from staff operating at the top of their skill sets/focusing on meaningful patient interactions rather than routine transfers. The system maintains a 92% employee retention rate with 3.9 median tenure in the access center department.
Conclusion: The $995,000 Question
This Southern New Jersey health system’s success reveals critical insights every healthcare leader must understand about the evolving communication landscape. Contrary to executive assumptions, younger patients haven’t abandoned phone communication—they’ve elevated expectations for what phone service should deliver. “Gen Z has substantial lack of patience,” notes one patient access executive. “They don’t want to waste time trying to solve a problem online if they know they need to talk to a person. But if you make them wait on hold, they will hang up. You get one, maybe two shots to serve them well.”
Unlike older generations with established physician relationships, younger patients switch providers without hesitation. Poor phone experiences don’t just frustrate them—they drive them to competitors.
The broader strategic implications extend beyond operational improvements. This health system’s CEO emphasizes, superior consumer experiences translate directly to financial benefits: better patient acquisition, retention, engagement, and reduced administrative costs. Voice channel modernization isn’t optional — it’s competitive survival.
Amazon, CVS, and other consumer-focused companies entering healthcare bring sky-high service expectations. Patients experiencing frictionless customer service in retail and hospitality won’t accept outdated phone systems from healthcare providers.
The path forward is clear for healthcare CIOs and executives. Don’t ignore the phone in healthcare — because your patients, from the youngest to oldest generations, certainly haven’t. They’re using it, they need it, and they’re judging your entire organization by how well you answer it.
This $3B health system partnered with Parlance to fix their outdated phone problem in 90 days, delivering measurable ROI that continues compounding. The question for other healthcare leaders is simple: healthcare leaders is simple: what are you waiting for?
Quantifiable Results
The outcomes are real and measurable:
- Parlance engages over 80+% of callers effectively.
- UW Medicine: Parlance IVR handled almost 4 million calls in the last year – 3,941,303 to be exact. The average self-serve rate was 84.3% and the average offload was 87.9%!
- UW Medicine: Parlance IVA handled 749,700 calls in the last year, with an average self-serve rate of 87.2% and an average offload of 91.1%!
- HCA Enterprise: Parlance IVR handled over 11 million calls in the last year – 11,131,519 to be exact. The average offload rate across all divisions and applications was 65%
- Virtua Health: Press Ganey patient satisfaction improvement metrics showed a 13%. increase in Ease of Contact and a 29% increase in Ease of Scheduling within 9 months. Self-service grew from 51.5% to 68.2% of all calls. Virtua’s net promoter score climbed from 20 to 55 after Parlance was implemented at the health system’s digital front door.
- One midsized health system with 11 hospitals and 1.5 million annual calls realized these outcomes: $1,456,800 in annual cost reduction, 6,070 monthly agent hours saved in their first live month, and 18 weeks of equivalent human labor recovered in the initial 30-day period.
- One major healthcare system saved the equivalent of 45 weeks of labor in a single month, after implementing Parlance.
Quantifiable Results
The outcomes are real and measurable:
- Parlance engages over 80+% of callers effectively.
- UW Medicine: Parlance IVR handled almost 4 million calls in the last year – 3,941,303 to be exact. The average self-serve rate was 84.3% and the average offload was 87.9%!
- UW Medicine: Parlance IVA handled 749,700 calls in the last year, with an average self-serve rate of 87.2% and an average offload of 91.1%!
- HCA Enterprise: Parlance IVR handled over 11 million calls in the last year – 11,131,519 to be exact. The average offload rate across all divisions and applications was 65%
- Virtua Health: Press Ganey patient satisfaction improvement metrics showed a 13%. increase in Ease of Contact and a 29% increase in Ease of Scheduling within 9 months. Self-service grew from 51.5% to 68.2% of all calls. Virtua’s net promoter score climbed from 20 to 55 after Parlance was implemented at the health system’s digital front door.
- One midsized health system with 11 hospitals and 1.5 million annual calls realized these outcomes: $1,456,800 in annual cost reduction, 6,070 monthly agent hours saved in their first live month, and 18 weeks of equivalent human labor recovered in the initial 30-day period.
- One major healthcare system saved the equivalent of 45 weeks of labor in a single month, after implementing Parlance.